What is Sleep-Disordered Breathing?
Snoring and OSA are some of the most common sleep disorders.
What is Sleep-Disordered Breathing?
Sleep-disordered breathing (SDB) describe a group of disorders characterized by abnormalities of the respiratory pattern or ventilation during sleep.
They include:
-
- OSA disorders
- OSA, adult
- OSA, pediatric
- OSA disorders
-
- Central sleep apnea syndromes
- Central sleep apnea with Cheyne-Stokes breathing
- Central sleep apnea dur to medical disorder without Cheyne-Stokes breathing
- Central sleep apnea due to high altitude periodic breathing
- Central sleep apnea dur to medication or substance
- Primary central sleep apnea
- Primary central sleep apnea of infancy
- Primary central sleep apnea of prematurity
- Treatment-emergent central sleep apnea
- Central sleep apnea syndromes
-
- Sleep-related hypoventilation disorders
- Obesity hypoventilation syndrome
- Congenital central alveolar hypoventilation syndrome
- Late-onset central hypoventilation with hypothalamic dysfunction
- Idiopathic central alveolar hypoventilation
- Sleep-related hypoventilation due to medication or substance
- Sleep-related hypoventilation due to a medical disorder
- Sleep-related hypoventilation disorders
-
- Sleep-related hypoxemia disorder
- Sleep-related hypoxemia disorder
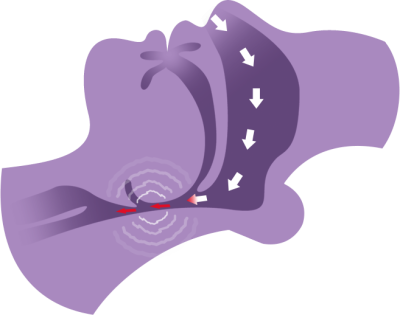
Snoring and OSA are some of the most common sleep disorders. In most cases, snoring and OSA are caused by a loss of muscle tone in the airway leading to noisy vibrations (snoring) and/or airway collapses (obstructive sleep apnea, OSA) (Figure 1).
OSA is the complete (apnea) or partial (hypopnea) reduction in airflow through the upper airways requiring an arousal to regain muscle tone and allow normal breathing to resume.
Untreated snoring can reduce sleep quality for the snorer and their bed partner. It may cause:
- Daytime drowsiness
- Irritability
- Impaired cognitive function
- Decreased libido
- Psychological/relationship issues.
Untreated OSA can lead to significant daytime sleepiness and increased risk of motor vehicle and occupational accidents. The continual physiological stresses of upper airway obstruction have also been shown to increase risk of:
- High blood pressure
- Atrial fibrillation
- Heart failure
- Stroke
- Type 2 diabetes.3
Sufferers of severe OSA may wake regularly during the night gasping for breath. Being overweight or having a large neck size can increase airway collapsibility. Alcohol and drug use can also increase relaxation of soft tissues and worsen the effect.
The estimated economic cost of undiagnosed OSA was nearly $150 billion in USA in 2015. This is greater than asthma, heart failure, stroke and hypertensive disease. It would cost $49.5 billion to diagnose and treat every American adult who has OSA. However, this expenditure could produce savings of $100.1 billion (Figure 3)4
Figure 3: The economic cost of undiagnosed OSA in USA.
Figure 4: The unmet need: the opportunity for dentists 1,2,4,5
How can Dentists Help?
Dentists play a pivotal role in the identification and treatment of obstructive sleep apnea. They see around half the population every year and are well placed to identify oral signs and symptoms.
Dentists can easily screen their patients, often starting a conversation with a simple question like “Do you snore?”.
Dentists are also responsible for one of the two leading treatments for obstructive sleep apnea, mandibular advancement devices (MADs). After patients are diagnosed with OSA by a physician, the dentist will fit and adjust the MAD but also carefully monitor potential dental side effects and collaborate with the physician to confirm ongoing treatment effectiveness. This can be highly rewarding work for a dentist; an opportunity to treat a debilitating medical condition and to change patients’ lives.
There are vast numbers of patients in need of diagnosis and treatment (Figure 4) but current secondary care infrastructure is inadequate to meet the need. The latest estimates suggest that there are nearly 80 million people in USA alone with mild to severe OSA2 but only ~6 million have been diagnosed4. This means that each of the ~7,500 board-certified sleep specialists in USA5 would need to identify and treat an average of 10,000 new patients from their local population to successfully meet the public health need. Dentists can significantly reduce this backlog by screening and treating patients in their practices.
Common signs and symptoms of OSA include:
- Loud snoring that disturbs others
- Daytime sleepiness
- Drowsiness while driving
- Frequent waking and/or need to urinate at night
- Choking or gasping during sleep
- Morning headaches
- Irritability and depression due to sleepiness and fatigue
- Elevated blood pressure that is difficult to control
The American Academy of Sleep Medicine (AASM) recommends asking all adults if they are dissatisfied with their sleep or have daytime sleepiness as part of routine health evaluations. Validated questionnaires are used to make a first screening assessment of patients suspected of obstructive sleep apnea. These include:
Epworth Sleepiness Scale (ESS)
Simple home testing devices based on the measurement of blood oxygen (oximetry) or peripheral arterial tone (PAT) are also sometimes used by dentists to gain a more objective screening result.
After screening a patient, taking their medical and dental history and completing an oral exam, dentists will refer patients who snore or are suspected of having OSA to a sleep centre, sleep physician or sleep testing service (Figure 5).
Figure 5: Typical pathway for patients screened and treated for snoring or obstructive sleep apnea by dentists (varies by country).
AASM and AADSM recommend that a diagnostic assessment should be conducted by a board-certified sleep physician for all patients suspected of having OSA and these evaluations are increasingly conducted using at-home diagnostic and telemedicine techniques. This means that a patient initially screened by a dentist can often be assessed quickly by a physician before returning to the dentist for treatment with a MAD if appropriate.
The diagnostic assessment often includes objective testing using a home sleep apnea testing device (HSAT) which measures airflow, blood oxygen, heart rate and thoracic movement. The severity of OSA and excessive daytime sleepiness must be determined before initiating treatment, not least to guide selection of the most appropriate treatment, but also to provide a baseline against which the effectiveness of future treatments can be measured.
If the patient has a complex medical history, it may not be appropriate for them to undergo sleep testing at home and they may need to attend a sleep clinic overnight for a more comprehensive polysomnography (PSG) assessment. This will be determined by the attending medical professional.
OSA severity is often graded according to the average number of apnea and hypopnea events that occur per hour of sleep.
- An apnoea is defined as a decrease in the amplitude of the respiratory flow ≥ 90% for 10 seconds or more.
- Obstructive Sleep Apnea is a mechanical problem that implies persistent respiratory efforts.
- Central Sleep Apnea is a neurological condition, that implies the absence of respiratory efforts.
- Mixed Apnea is a neurological condition followed by a mechanical problem. It implies the absence of respiratory efforts followed by persistent respiratory efforts.
- An obstructive-hypopnoea is defined as:
- a decrease in the amplitude of the respiratory flow ≥ 50% of at least 10 seconds
- or a decrease in the amplitude of the respiratory flow ≥ 30% of at least 10 seconds
- with oxygen desaturation of at least 3%
- or micro awakenings measured by electroencephalogram
- or automatic micro awakenings that can be linked to an increase of the pulse of at least 5 beats per minute.
An apnea-hypopnea index (AHI) measures sleep apnea severity. AHI is calculated by adding together the number of apnea and hypopnea events and dividing by the number of hours of sleep.
| Apnea-Hypopnea Index (AHI)1 | |
|---|---|
| Mild Sleep Apnea | AHI of 5 to 15 |
| Moderate Sleep Apnea | AHI of 15.1 to 30 |
| Severe Sleep Apnea | AHI > 30 |
Central sleep apnea (CSA) is another SDB condition with similar symptoms to OSA but is not caused by an obstructed airway. CSA is a relatively uncommon central nervous system disorder in which the body’s neurological trigger to breathe during sleep does not function correctly. Mixed sleep apnea (MSA) is a combination of OSA and CSA.
It is important to rule out CSA as part of the diagnostic assessment before treating a patient with a device that acts on an obstructed airway.
Treatments
Treatment guidelines vary by country, depending on local policies and reimbursement rules. CPAP, MADs and lifestyle changes are the primary treatments recommended for snoring and obstructive sleep apnea. For more information about local practices, see the Useful Resources and Recommended Reading.
Lifestyle Changes
Changes in lifestyle or behavior, such as such as losing weight, cutting back on the use of alcohol or sedatives and avoiding sleeping in a supine position, may also be suggested as a treatment for snorers or as an adjunctive treatment for patients receiving CPAP or a MAD.
Continuous Positive Airway Pressure (CPAP)
Continuous Positive Airway Pressure (CPAP) is recommended as the first-line treatment for severe OSA. CPAP treatment involves wearing a mask during sleep which is connected to a device that pushes air into the airway. It is a very effective treatment when in use. The airway pressure splints open the airway (pneumatic splint), holding it open throughout the night with positive airway pressure.
However, CPAP can be difficult to tolerate due to poor fitting or uncomfortable masks, nasal congestion, dry airways and difficulty adapting to the air pressures. Adherence to CPAP is affected by many factors including disease severity, anatomical features, and degree of clinical support.
Adherence varies substantially across different settings; it has been reported that between 29% and 83% of patients enrolled in research studies use CPAP < 4 h per night.6 A systematic review of 66 clinical trials and cohort studies published between 1994 and 2015 found a weighted average adherence of 4.5 h per night, with no meaningful improvement discernible over two decades.7

Figure 6: MAD treatment; mechanism of action
Mandibular Advancement Devices (MADs)
MADs are oral appliances that treat snoring and obstructive sleep apnea by holding the mandible in a forward position, thereby increasing space in the airway and decreasing airway collapsibility (Figure 6).
The implementation of MAD therapy and the medical and dental follow-up are often the result of a collaboration between a sleep specialist and a dental practitioner. To maximize tolerability and minimize risk of tooth movement, injury to the TMJ, muscle pain, gum irritation, etc. Panthera’s D-SAD devices are an excellent example of custom-made MADs whose designs have been refined over many years to achieve these objectives effectively.
CPAP versus MAD
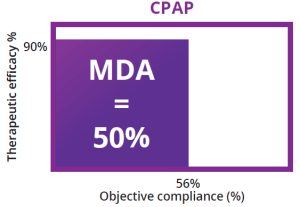
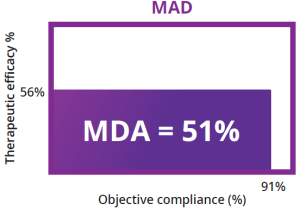
CPAP has been shown to be more effective than MADs at reducing OSA severity when in use. However, MADs are generally better tolerated by patients and are therefore used for more hours of the night (they are associated with better adherence). Since both therapies are only effective when in use, the mean disease alleviation (MDA) of these two therapies is therefore very similar.
MDA is calculated by plotting compliance and therapeutic efficacy (AHI baseline minus AHI with therapy applied, expressed as a percentage). In a pivotal study by Vanderveken et al. MAD treatment was shown to reduce the mean AHI by 56% from baseline with an adjusted compliance (objective MAD use adjusted for the total sleep time) of 91%. Consequently, the MDA was 51%.10
Since CPAP is more effective at reducing OSA severity but has lower compliance, the MDA of these two treatments has been shown to be equivalent (Figure 7).11
Therapeutic options: The role of MAD
The latest joint AADSM and AASM practice guidelines recommend that sleep physicians should prescribe oral appliances (rather than no therapy) for adult patients with primary snoring and/or obstructive sleep apnea who are intolerant of CPAP therapy or prefer alternate therapy8.
In the United States, the Centers for Medicare and Medicaid Services (CMS) and most private insurances will reimburse MADs as a first-line treatment for patients who are:
- Diagnosed with mild OSAHS (AHI 5-14 with daytime symptoms or co-morbidities).
- Diagnosed with moderate OSA (AHI or RDI 15-30).
- Diagnosed with severe OSA (AHI or RDI >30) and who are contraindicated for CPAP.
MADs are also reimbursed as a second-line treatment for patients who are diagnosed with severe OSA (AHI or RDI >30) and who are unable to tolerate CPAP.9
The Opportunity
The scale of the opportunity to improve lives with oral appliance therapy (OAT) is considerable:
CPAP non-compliant
50% of patients receiving CPAP treatment for OSA are non-compliant after 6 months and 83% are non-compliant after 5 years.5
Half of adults snore
Around half of adults snore, many of them habitually.1 Untreated snorers often develop OSA.
Untreated OSA
Untreated OSA causes daytime drowsiness and increases risk of high blood pressure, atrial fibrillation, heart failure, stroke and type 2 diabetes.3
Oral appliances opportunity
Oral appliances are a first-line treatment for snoring and mild to moderate OSA and a second-line treatment for severe OSA when CPAP is contraindicated or can’t be tolerated.8,9
Starting Out in Dental Sleep Medicine?
The scale of the opportunity to improve lives with oral appliance therapy (OAT) is considerable.
What is Sleep Bruxism?
Sleep bruxism is a parafunction in which the masticatory muscle activates involuntarily during sleep. Sleep bruxism can be diagnosed in a number of ways.